The Affordable Care Act requires coverage for pediatric vision care as one of the essential health benefits. The ACA does not require insurers to provide routine vision care coverage for adults.
For children under the age of 19, vision coverage is included in all new small group and individual health insurance plans (with effective dates of January 2014 or later), on and off-exchange. This means kids have coverage for eye exams, vision screening, and glasses to correct vision problems.
The specific pediatric vision services that must be covered by individual and small group plans will vary from state to state, depending on the benchmark plan the state uses. In most states, the benchmark plan’s pediatric vision coverage includes one annual eye exam and one pair of glasses, including frames, per year. (“Covered” doesn’t mean covered at no cost. There can be copays, deductibles, and coinsurance for these services.) You can see updated benchmark plan information for each state here.
Vision screening for children falls under the category of preventive care, which means it’s covered at no charge until kids turn 19 (as long as you have an ACA-compliant plan).
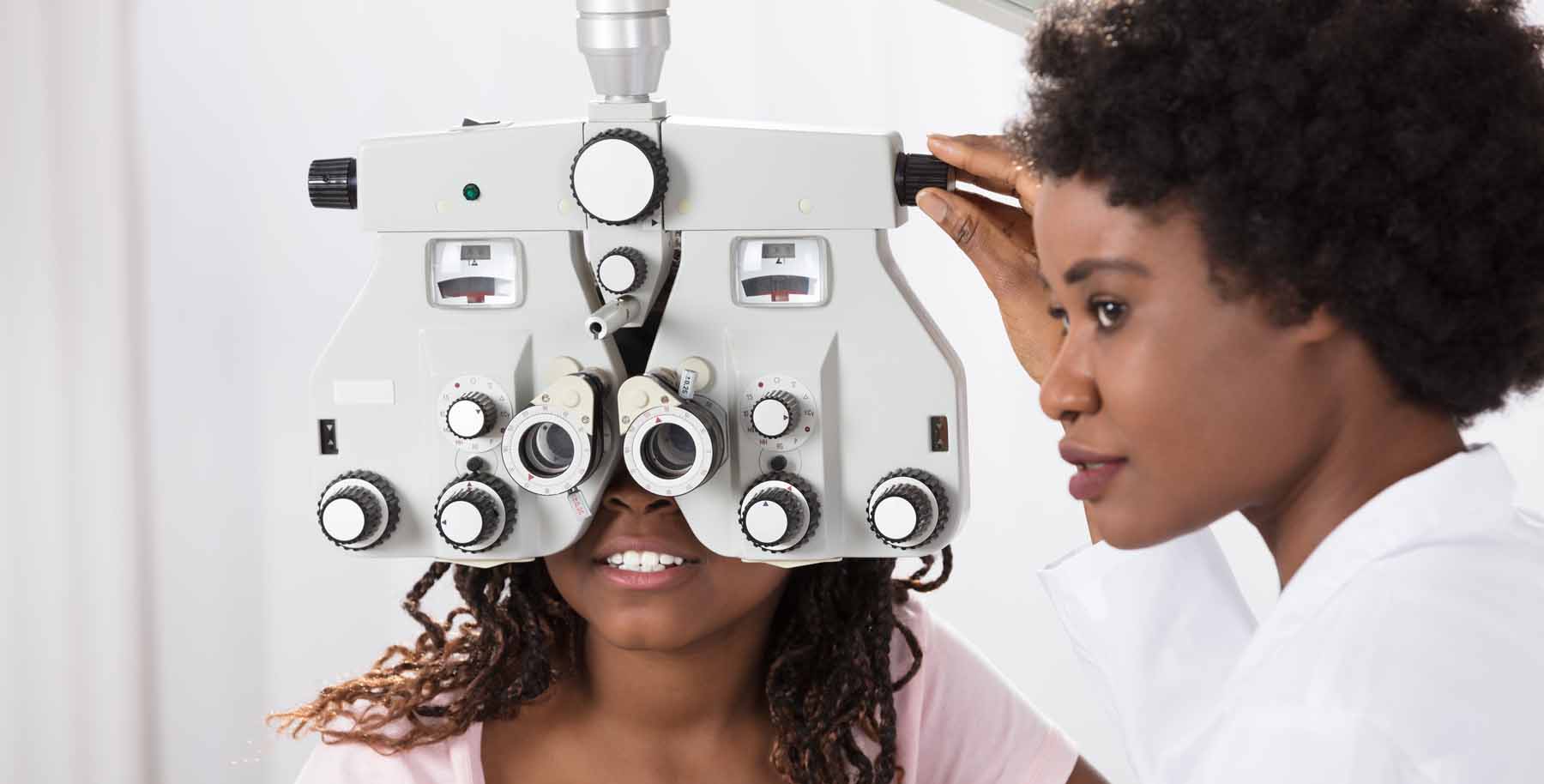
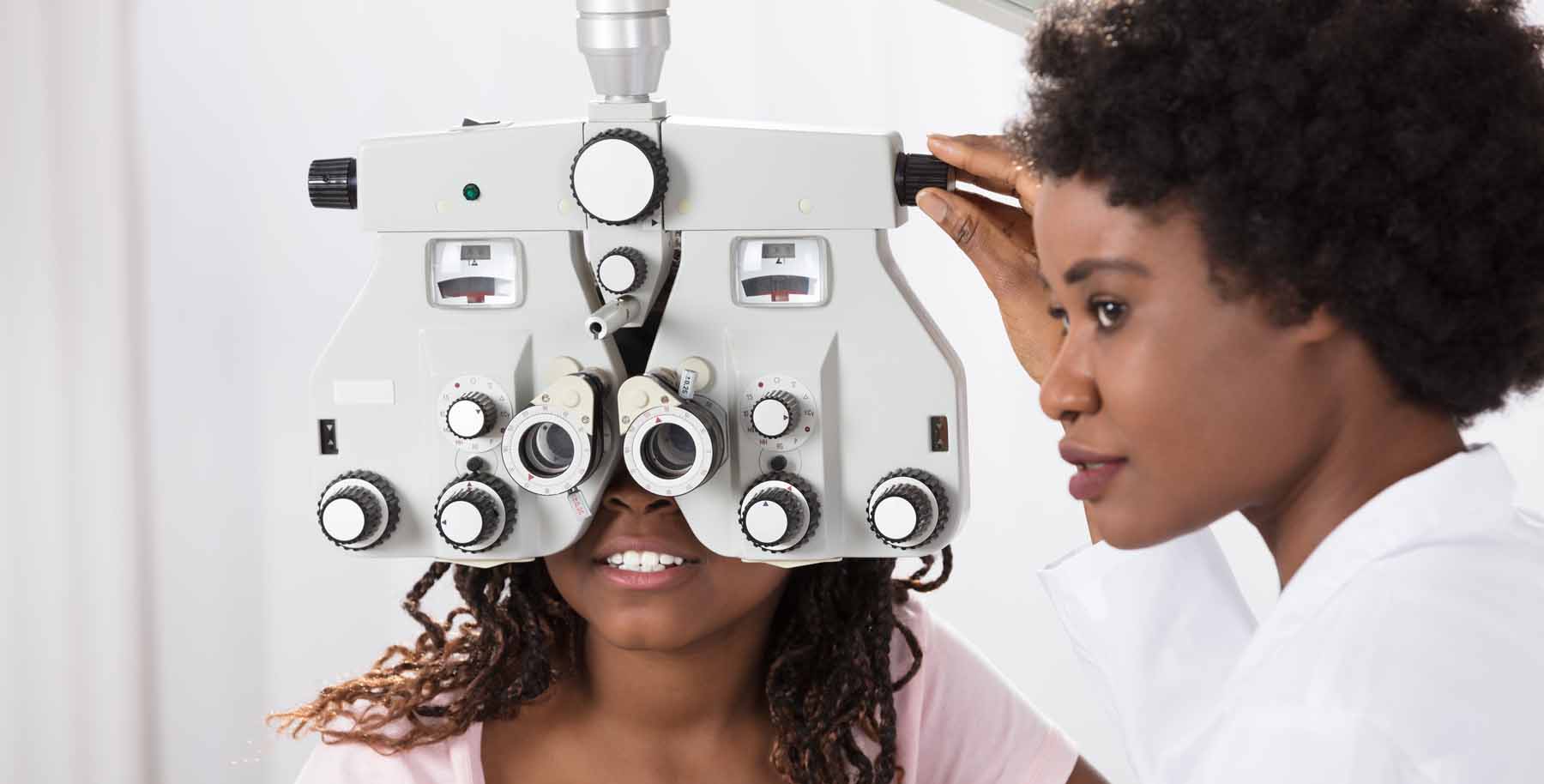
But vision screening is not the same thing as an eye exam. Vision screening can be performed by a pediatrician or family physician to identify or detect vision difficulties. The screening may not diagnose the child’s condition, but it can indicate whether the screening should be followed up with a comprehensive exam.
Although pediatric vision care beyond vision screening is covered under the ACA, everything other than vision screening can have copays, or be counted towards the deductible and/or covered with coinsurance. So although the eye exam will be covered as part of the ACA’s pediatric vision coverage, the cost-sharing specifics will vary from one plan to another. Some carriers do offer free eye exams and glasses for kids though – it depends on the carrier, so read the fine print on the plans you’re considering.
In general, corrective contact lenses for children will be covered by individual and small group plans. But the specifics will vary from state to state, depending on the details of the state’s essential health benefits benchmark plan. Some will distinguish between elective contact lenses and medically necessary contact lenses. Some will only cover a partial-year supply of contact lenses. Some will only cover contact lenses in lieu of glasses, so a family would not be able to have coverage for both within the same year.
It’s also common for contact lenses to be subject to the health insurance deductible. This means that the family would pay the full cost (after the health plan’s network-negotiated discount) if the deductible had not yet been met for other services earlier in the year. After the deductible, the health plan would pay a portion of the cost of contact lenses (assuming this is a covered benefit), subject to the plan’s coinsurance.
Routine vision care coverage is not mandated for adults by the ACA. Health plans can opt to include adult vision coverage in their benefit design, but they are not required to do so.
If your employer offers health insurance, there’s a good chance that vision coverage is included in your employee benefits package. If it’s not, you can purchase a stand-alone vision plan. Depending on how much vision care you use, it may or may not make financial sense to do so.
If the health plan you’re considering – on or off-exchange – doesn’t include adult vision coverage, you may want to purchase a stand-alone adult vision plan. In most states, stand-alone vision plans are not offered through the exchanges, and even if they are, you can’t use your premium subsidy to offset their cost.
HealthCare.gov (used in 33 states as of the 2023 plan year) does not offer any stand-alone vision plans. But several of the fully state-run exchanges have established partnership arrangements with a stand-alone vision coverage company (VSP, in most cases: California, Colorado, DC, Idaho, Kentucky, Maryland, and Nevada). In these states, visitors to the exchange are directed to a link where they can purchase stand-alone vision coverage directly from the vision coverage provider.
When we talk about vision coverage, we’re generally referring to optometry care. This involves the process of vision testing and correction, and is generally not covered under health insurance plans for adults.
However, ophthalmology services to treat eye injuries, illnesses (such as cataracts or macular degeneration), or infections would generally be covered by health insurance policies, subject to the same cost-sharing as other medical conditions. It’s also common for health plans to cover (subject to normal cost-sharing) one pair of glasses following treatment for cataracts or an accident that damaged one or both eyes.
Note that although LASIK surgery is done by ophthalmologists, it is almost never covered by self-purchased health insurance; LASIK falls under the category of vision correction, rather than treatment for an injury or illness that’s affecting the eye.
If you’re buying ACA-compliant individual health insurance (on-exchange or off-exchange), or enrolling in an ACA-compliant small group health plan, pediatric vision coverage will be included in the plan, as described above. But keep in mind that the plan’s regular deductible and coinsurance can apply to any services beyond vision screening (which is not the same thing as an eye exam).
If your employer offers separate vision coverage as part of your benefits package, they will likely pay part of the premium, making your monthly cost for the coverage quite low.
If you want to buy your own adult vision coverage, you’ll find plans with monthly premiums under $15 per person, although plans with enhanced benefits can be more than $30/month. Stand-alone adult vision plans generally cover one annual eye exam with a low copay ($15 is common), and will provide an annual allowance for frames and lenses or contact lenses (a $150 allowance is common on basic plans, but more expensive plans will generally pay a higher amount).
Original Medicare (Medicare Parts A and B) does not include coverage for routine vision services. Coverage is provided for eye diseases and injuries, so Medicare will, for example, pay for cataract surgery (subject to the normal cost-sharing requirements; in most cases, this means the Part B deductible and coinsurance).
Virtually all Medicare Advantage plans provide at least some coverage for eye exams and eyeglasses, although the specifics will vary from one plan to another. There’s a lot to consider when deciding between Original Medicare and Medicare Advantage (here are several things to keep in mind). The vision benefit would be a very small part of the big picture, but it is something to take into consideration.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.